How to Empower Ourselves to Better Health
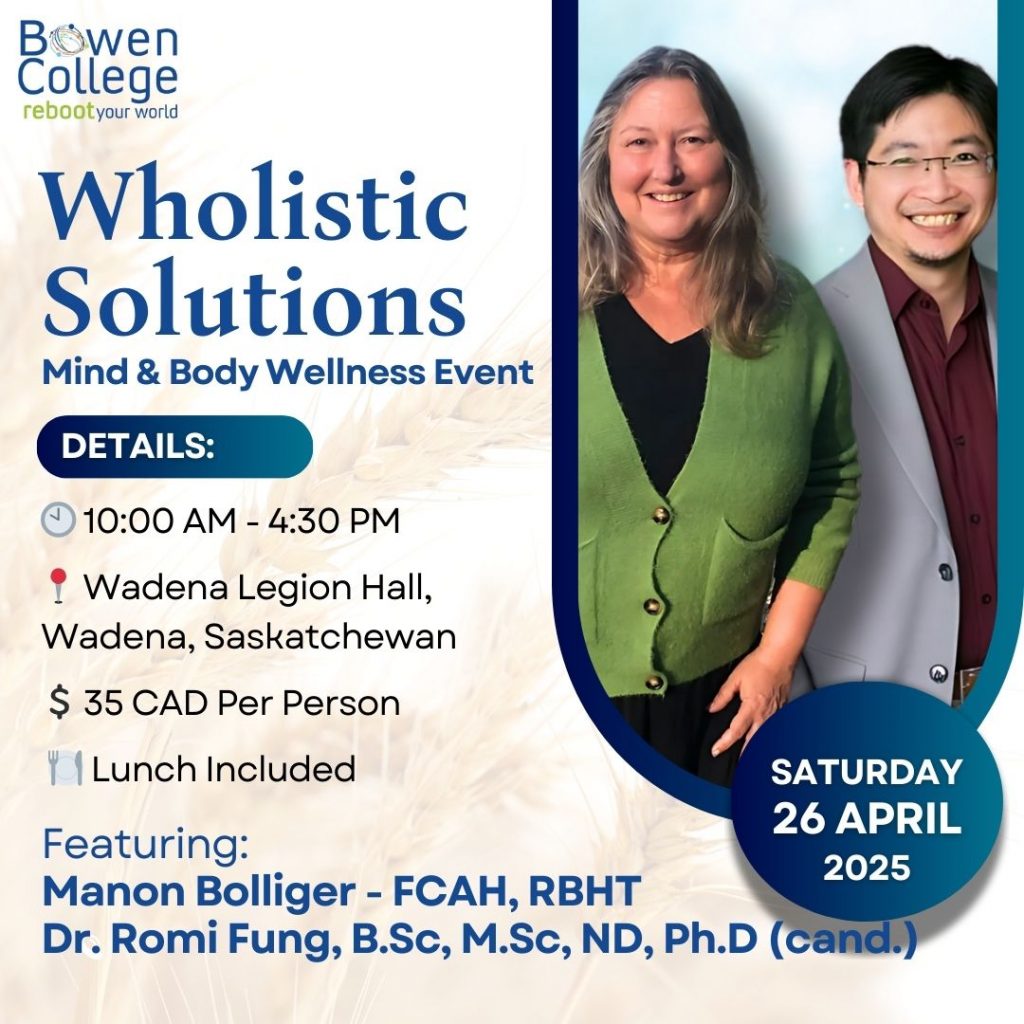
with Dr Hamid Elmyar on The Healers Café with Dr. Manon Bolliger, ND
In this episode of The Healers Café, Dr. Manon Bolliger, ND, chats with Dr Hamid Elmyar, CEO, Podcast Host, is a Fulbright scholar, and speaks multiple languages
Highlights from today’s episode include:
Dr. Hamid Elmyar 11:21
My philosophy in life is that power is in empowering others. As far as we have that in mind that to empower other people. And that’s why I see the root causes when I mentioned a couple of problems, and in those communities, preventable diseases such as diarrhea, and bronchitis. There were other diseases, also preventable diseases, but lack of education, unfortunately, lack of awareness about health issues. And that those are the main causes, the root causes, lack of access to quality health, lack of basic education like illiteracy, and socioeconomic status. These all play an important role in people’s health across the world, and especially in developing countries.
Dr. Hamid Elmyar 19:16
I realized that the healthcare professionals, unfortunately, especially during this pandemic time, also suffer somehow from the burden and burnout, and that’s a major issue. If the healthcare professionals are not happy, what they do and they are not healthy and satisfied with the job that they’re doing, then definitely it affects their productivity. It affects the way that they treat their patients
Dr. Hamid Elmyar 42:43
So the message is most of the belief that I have is that health is not limited to private practices in hospitals. It has to start from every individual communities, school systems, everywhere. And for that to happen, we need to raise awareness, we have to look for those underlying causes and root causes. And we have to have a collaborative, systematic approach to health in order to save people’s lives. Also, not only helping our communities but health care professionals themselves as well.
About Dr Hamid Elmyar:
Hamid Elmyar, M.D. earned a master’s degree; from Montclair State University, Montclair, New Jersey. As a medical professional having experienced firsthand the devastating consequences resulting from a lack of accessible public health education and awareness which often led to the unnecessary loss of life in his country of origin, Afghanistan, he decided to immigrate to the United States where he has made it his mission to bring public awareness to a worldwide audience.
He hosts a biweekly podcast, “With Dr. E”, which invites experts in health, education, and community development from around the globe to share their experience, knowledge and insight with the world. Recently, his program has highlighted the experiences of those confronting the current coronavirus pandemic and the resultant socioeconomic implications to better understand what effective leadership is and how it can help mitigate this health crisis.
Dr. Hamid Elmyar believes health is not limited to private practices and hospitals; it has to start from every individual. He is known for bringing world’s health professionals from all specialties around the same table for an upstream approach to health in order to impact millions.
He strongly believes the insight and experiences of some of the world’s renowned leaders in clinical and public health should be shared broadly and his podcast aims to promote and facilitate this.
Dr. Elmyar is a Fulbright scholar, speaks multiple languages and resides in New Jersey.
My core purpose and philosophy in life is to empower and transform healers and communities. Because I believe that power is empowering others.
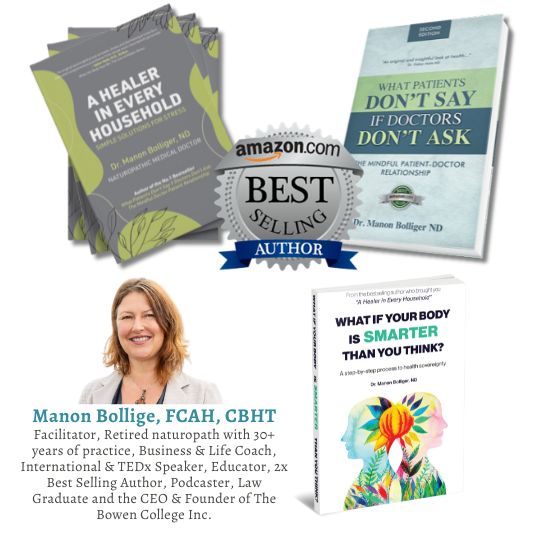
About Dr. Manon Bolliger, ND:
Dr. Manon is a Naturopathic Doctor, the Founder of Bowen College, an International Speaker with an upcoming TEDx talk in Jan 2021, and the author of the Amazon best-selling books “What Patient’s Don’t Say if Doctors Don’t Ask” and “A Healer in Every Household”.
SOCIAL MEDIA:
Dr. Manon, ND – Facebook | Instagram | LinkedIn | YouTube | Twitter
About The Healers Café:
Dr. Manon’s show is the #1 show for medical practitioners and holistic healers to have heart to heart conversations about their day to day lives.
Follow us on social media! https://www.facebook.com/thehealerscafe
TRANSCRIPT
Dr. Manon 00:03
So hello, and welcome to the Healers Cafe. And today I have with me, Dr. Hamid Elmyar. And we met during another conference, and I just fell in love with his story and his passion. So it’s really a great pleasure to have you here on the show. So I understand that you went from being a doctor into public health. And I wondered if you could just sort of explain how your life unfolded on that level?
Dr. Hamid Elmyar 00:41
Well, absolutely. Thank you so much. First of all, it’s a pleasure to be on your show, Dr. Manon and, of course, we met at that event, and I really appreciate what you’re doing for humanity in general. Thank you so much for having me on your show. Starting with my story and myself, why do I do what I do and why? From early childhood, it may sound just cliche, but it’s true that from early childhood, I always wanted to help people. And in order to help people, I was looking for ways that I have to finish school, you know, have to do my education, so that I can be more helpful. And so after finishing high school, I was thinking about a way to help people and what would be better than, just going to med school. And I’m originally from Afghanistan, I was born and raised there in Afghanistan. And as many of your audience and yourself know that Afghanistan, unfortunately, is one of the countries that has been suffering for decades now. In terms of security, in terms of lack of health care facilities, as well as education and everything. And in that community, that I was brought up in, I was lucky enough to finish my school, even during this hard time, where people were not even able to go to school, sometimes I was just going into school. And that’s a totally different story.
Dr. Hamid Elmyar 02:36
How, if your time allows, on your show, I can tell you a little bit of that experience in my childhood. That we had basically, we didn’t have classes like here in the Western countries in Europe, or in America or Canada. We had classes which my class was a tent, I was studying under a tent. And we didn’t have any chairs, we didn’t have desks, we were sitting on the floor with a tarp on the floor, sometimes that. Sometimes even it was raining, it was coming on under the tent. We had to just sit on our feet with shoes on. And part of my classes during my childhood was also in a bus wreckage, like just a broken bus, with no tires, nothing. But we were using that in our school as a classroom. And the days that our class wasn’t on that bus, broken bus, I was so happy that today we are not there on that bus. So that’s how I was studying during my early childhood. And, in primary school and finishing high school, I always wanted to help people so then I went to med school. Being the top student in my class during high school, it wasn’t that difficult for me to get into medical school. And so studied medical school for seven years back there, so after graduating, long story short graduating from medical school, I was just thinking that ‘Oh, now I am a physician, am I really able to help people?’ And soon I realized that no, this is not enough. If I want to help people, I have to specialize in something, I have to be more specific. Who am I working with and how can I be more helpful?
Dr. Manon 04:45
So can I just stop you there for a second? So you started with…
Read more...
this desire to help and then how did you get focused on health to start with like why health because you can help people in lots of things. So why was it health?
Dr. Hamid Elmyar 05:06
That’s a very good question. There were a couple of reasons, one was that, basically to health, if everything we do in this world is just to be healthy and to be happy, right? If it’s any type of work if you’re not healthy, you can’t do anything. That’s the bottom line. So I just was thinking that health is the best way to help people, and especially people who need it. Like patients and other people who need health advice, that would be a good way. The second reason was that back then in Afghanistan, unfortunately, a lot of other majors, like even journalism, or engineering or other ones, were not really…there was not an opportunity to, even if you studied that, to work. So I was thinking that if I go to med school, there’s always a need, apart from my passion, that you have to survive. So, those two reasons why I chose health.
Dr. Manon 06:16
Because it’s funny when you look at them. I also felt like I wanted to help. But it’s interesting that the first choice I had was law because I felt like you have to be able to protect people’s rights and their freedom of choice. So I went there, and then I realized, no, the only thing that will matter is from the ground up, from the roots up, is if people start to take charge of their health because that’s something that they can control. And it gets more complicated as time goes by, but we’ll go into that. So it’s interesting. What we get brought up with and why we get interested in how we help people. So anyway, so go on, so then you became a doctor…
Dr. Hamid Elmyar 07:07
Exactly, that’s a great point too. To know the laws and everything that’s important, too. So then I finished medical school, and I just was asking myself, am I really helping people? What am I able to do? And for that, I was also during my medical school, I was also doing part-time, community health outreach programs with an international organization back in Afghanistan. And that was also part of the reason I wanted to see where am I going? Am I going to clinical work or public health? So after medical school, and I said, “Maybe I should do a specialization and do a residency to be more helpful”. I did a residency in pediatrics, and so the reason also I chose pediatrics, because women and children, unfortunately, and across the world, especially in developing countries are the most vulnerable members of society. And I was seeing that need there in Afghanistan. So I did my residency in pediatrics, in order to be more helpful to people. Then it was during my third year, last year of residency in pediatrics, that was a life-changing time that as a senior resident. I was on call and I was an OPD with other physicians, we were seeing a lot of patients on a daily basis. I’m talking about the 100-150 plus patients, on OPD like three, four physicians. Which is really not the way it should be, and it’s not easy to do so. But many of those patients, kids will come in, of course, what their mom’s from underserved communities from that they were suffering, unfortunately, from very easily preventable, and diseases, preventable diseases, such as diarrhea, or bronchitis. And that was a moment I also was on call one night and I saw patients come in from remote areas, unfortunately, two, three days on the way and in critical conditions at the hospital. And when I was looking for the underlying cause, the underlying cause was diarrhea or some very easily preventable disease. And unfortunately, some of them couldn’t even make it because they came in irreversible shock and heart failure, renal failure, and all that. And that was a moment I was asking again, myself, like am I really helping people? Like I always wanted to help people, I did med school and then I did a residency in pediatrics now, am I really helping people? Why are these people getting sick in the first place? And why, are a majority of them are coming here from very easily preventable diseases? What are actually the underlying causes? What is the root cause?
Dr. Manon 10:23
No, I know because that’s a subject very dear to my heart, what are the root causes because they believe that we can take more charge and more responsibility for health. That doesn’t mean not working with a health advisor, or a doctor, or a health team. I’m not suggesting that, but it does start with having higher expectations of what’s possible for you, and then taking responsibility to act upon some of the things. So to me, if becoming knowledgeable enough, as a public, to be empowered, is very important. So I’m very curious what to you are the root causes, the real root causes?
Dr. Hamid Elmyar 11:18
Yes, absolutely. And I totally agree with you.
Dr. Hamid Elmyar 11:21
My philosophy in life is that power is in empowering others. As far as we have that in mind that to empower other people. And that’s why I see the root causes when I mentioned a couple of problems, and in those communities, preventable diseases such as diarrhea, and bronchitis. There were other diseases, also preventable diseases, but lack of education, unfortunately, lack of awareness about health issues. And that those are the main causes, the root causes, lack of access to quality health, lack of basic education like illiteracy, and socioeconomic status. These all play an important role in people’s health across the world, and especially in developing countries.
Dr. Hamid Elmyar 12:08
So when I was looking for the underlying cause, why’d that specific patient with diarrhea that came in a critical condition? When I looked for the underlying cause, first of all, the entire family was illiterate, so they couldn’t even read and write. So basically, they didn’t know any, they didn’t have any information or enough information about diarrhea. About basic personal hygiene and environmental hygiene, and what would be…how would it be possible for them to prevent it? And even when someone’s suffering from the area, the basic things that you can give to a kid to help them restore and rehydrate, restore that energy, and rehydrate. I could sense the lack of such information among communities.
Dr. Manon 13:05
It’s information but is it also access, as in not easy access to water, and to sources that are not contaminated? Like we have these in the States, I’m from Canada, but I’ve interviewed several doctors who talk about these food deserts. I think they’re all bad. And it sounds like all there is fast food. There is no, there’s not one green vegetable, there is not anything of value, there are only chemicals and junk in it. And if that’s what food is, then how can food be your medicine? You’re destroying your health, but if you don’t have the basics like water, like clean water, then you have really nothing to the pillars, the building blocks of health are missing.
Dr. Hamid Elmyar 14:02
Absolutely. I can compare later on like how the US compared to the developing countries. Obviously, in developing countries, it’s not much of a fast-food thing because we don’t even have McDonald’s there in Afghanistan or in maybe around some other developing countries or some other fast food like that or change like that. But lack of, as you said, drinking water is one issue. There are places that they don’t have access to water. Most places would just dig a well in their backyard, or front yard and they just pull some water out of there in a bucket and drink it that way. There are people who don’t even use, like maybe just some elite families would be probably using, bottled water or something like that or they have a kind of the water system that can provide them with water. But mostly it’s just that type of water and there are places in the rural areas, probably they don’t even have that well, which is a little safer than, but then they just go to the river and get some water out of the river and drink it that way. So basically that water source is very important and like the vegetables that they use. Many probably don’t even know how to wash it or use some sort of like chemicals that they can kill the bacteria or the problem germs in there.
Dr. Hamid Elmyar 15:54
But to answer your question, it’s both information and systematic obstacles that can cause those diseases. By systematic obstacle, I mean, there are not enough healthcare facilities, there’s not enough even physicians or health care providers to provide the necessary information for people. And of course, lack of access to quality health is another major issue. So for that point, that was a point at the time that I wanted to help people as a pediatrician and then realized all those root causes. And I was looking again, for some other way to help people because that was not my answer. And for that to happen, I was looking for underlying causes, and just decided to do a master’s in public health and because then I would be happy and able to reach a population level. Rather than just sitting in my private practice, we’re at a hospital and seeing patients who are, unfortunately, already suffering from disease, and they have to spend a lot of money and resources. And then you don’t even know if they get well or not because of the quality of medications and compliance in those countries. So I decided to do a master’s in public health, and I applied also for a scholarship. I would say that I was lucky, and of course, my hard work paid off to get that and I did my Master’s in Public Health and focus on community health education here in the US. And I always, that’s another story when you were talking about the US health and food deserts and stuff like that before.
Dr. Hamid Elmyar 17:55
Even coming to the US, I was thinking that there are no public health issues here in the US and realize that, no, there’s definitely a lot. So that’s what I do now. I focus mostly on community health education, community health, and public health, and reaching a population level, rather than just clinical work.
Dr. Hamid Elmyar 18:19
But meanwhile, I also volunteer with a couple of nonprofits where I do also community health education. I also work in a diagnostic lab. It’s a pathology lab that we also diagnosed diseases, including COVID. And now that during this pandemic, so I am still thinking that’s another story, but we can probably discuss it later or another podcast. That would be my focus when I focus now mostly on healthcare professionals, because when I was looking to help people, so I did that, and I don’t want to repeat my story, again, medical school, seven years and then three years of residency in pediatrics in two years and Masters in Public Health. And now,
Dr. Hamid Elmyar 19:16
I realized that the healthcare professionals, unfortunately, especially during this pandemic time, also suffer somehow from the burden and burnout, and that’s a major issue. If the healthcare professionals are not happy, what they do and they are not healthy and satisfied with the job that they’re doing, then definitely it affects their productivity. It affects the way that they treat their patients. So my focus now in order to help people and communities, I need to make sure that the healthcare professionals are also healthy and happy and satisfied so that we can have a better approach from all walks of health. And that’s what I’m known for, to bring health professionals from all walks of health, around the same table from across the world to have an upstream approach to health so that we can have a successful approach to health.
Dr. Manon 20:21
Yeah, so I am in great agreement with you on that level, but where are you located right now?
Dr. Hamid Elmyar 20:30
Yeah, I am in the US. I’m in New Jersey, living in New Jersey, which is northeast US. And very close to New York. 20-30 minutes drive.
Dr. Manon 20:43
And what have you found, are the major stressors for the health care providers, because, I mean, I’m in Canada, I’m on the extreme other side? My clinic was in Vancouver, and I had many doctors and nurses that came to see me. And that was one of the big subjects of dissatisfaction and burnout, and not feeling able to perform and do what they know is right. So I’m just very curious, what have you found? In the States on the other coast entirely? What have you found from, and I know you interview people everywhere, on the subject? So what are the issues that you’ve noticed?
Dr. Hamid Elmyar 21:34
That’s a very good question. So before answering that specific question. I also host a podcast, and on my podcasts, I also interview physicians and healthcare professionals from around the world, to share their experience and knowledge, and insight with the rest of the world. And the burnout is, this is not specifically, I didn’t have any physicians talking specifically about this on my podcast, but what the conversations that I had with some physicians in my inner circle of friends, there is always that feeling of fatigue and tiredness and feeling of, you know, you don’t really have the work, life balance. I know, physicians who are working long hours, and they can’t really even find time to spend with the family and their loved ones, or let alone to go on vacation. And especially during this pandemic time, it’s been even tougher, because a lot of physicians, we needed them, and not only physicians, all healthcare providers, from nurses to other healthcare providers to be in the frontline. And so that that burden, feeling of tiredness and fatigue and not even satisfied what they do, because I always mentioned to my friends about the balance in life is just like, you go on to a gym, you work on all parts of your body, because you want to have that balance. You don’t want to work only on one arm, and then the other arm is disproportionate. That life and work are like that exactly. If it is physicians, if it is engineers, if it is, lawyers and other professions, there must be a balance in life. Your professional work, your personal life, your friends, and your social life. That’s another reason maybe a lot of…because, by nature, the health care profession is very demanding. I mean, it’s very tough, and we’re always working hard and competing against time.
Dr. Hamid Elmyar 24:09
I do have actually, sorry to interrupt, but I do have some statistics. And maybe later on, or whenever you want me I can tell you about the burnout.
Dr. Manon 24:22
Absolutely feel free. Because I would think that responsibility has also two edges. It’s like when you feel responsible, even if you’re the mother of a family or whatever, that possibility always has to be kept in check with self-care and teaching that part where the children learn that they need to respect that and they need their little time to sort their things out and make their own intelligent decisions. So it’s a microcosm of a bigger issue, but as Doctors, there are so many who feel responsible. And it’s not necessarily that the patient is going to follow, or can do, or will understand, or has enough time to even get the whole picture. Right? So it can be very frustrating but go ahead, what are the statistics you have found because I have not looked into this at all so?
Dr. Hamid Elmyar 25:22
Well, yeah, because I also work on the panel discussion that is focused on burnout among healthcare professionals. And I have some of the statistics in front of me here in 2013, the Medscape lifestyle report, surveyed 20,000 physicians, and reported nationwide in the US, 40% burnout among physicians in 2013. And then they did again in the 2017 report found 51% rate. So from 40 to 51%, in a matter of four years, there was a 25% increase. This is only one of the statistics. And this is, as I said, this was done in 2013 and 2017. Which, we all know that the burden now, because of the pandemic is way higher.
Dr. Manon 26:24
But what do you think? So it’s the life balance, which is a good thing. But I’m just wondering, and I’m looking at, in Ontario, I know the Ontario Nurses Association was very active, and they said to the government and to the people, ‘thanks for clapping at seven o’clock, that was great. We felt the support’. This is at the beginning of the pandemic when we really didn’t understand this virus and all that, but they said, and then they were trying to get cuts. They were offered cuts in their pay, and they’re saying no, wait a minute, here, it’s almost like when the pandemic peak rolled down, it’s almost like they don’t matter anymore. And so I look at that as a systemic problem, much larger than what the physician, the health care provider, the nurse, whichever, in the wellness team, what they can do, it’s a bigger picture.
Dr. Hamid Elmyar 27:36
Right.
Dr. Manon 27:37
And can you comment on that?
Dr. Hamid Elmyar 27:39
I do agree with that part, too. There’s, you know, part of it is on the physician or healthcare providers’ side, and then partly, it’s also with the providers of those facilities. In other words, decision-makers, and officials who are running those hospitals and governments and local governments, to provide them with the necessary equipment to make sure that they have the PPE and then to make sure that they have the support that they need. And, that was really surprising if they wanted to cut their payment, instead of increasing it. And, you know, just little bonuses that would be encouraging, not to mention that, unfortunately, a lot of physicians lost their lives and other health care providers across the world, in fighting this disease in order to help their patients and save their lives, but they put their lives at risk. And that emotionally is also another probably one of the contributing factors in burden and burnout when others you see a colleague or your senior doctor or mentor lost their lives in this pandemic. That is, of course, also other reasons that I agree with you on that.
Dr. Manon 29:12
Yeah. So what part of it do you feel, again, back to empowering in this case, the practitioner, the doctor, what are the things that they could do that’s not it’s not so obvious when you have crazy schedules. And when you’re not in charge of the decision making, you’re not in charge of some of the protocols that can be used or not used, even though it should be, we’ve seen that change with this pandemic, where they’re told this is how it’s done. And it’s like, Whoa, you know, so there’s been a lot of inner turmoil, but I would say there’s maybe during any sort of contagious time, there are definitely things that might be different. Because burnout is an issue outside of pandemics, too. So where do you see the nonvictim, because I prefer to think that we’re all agents and that we can actually actively make a change? Where do you see starting with that?
Dr. Hamid Elmyar 30:27
Well, that’s a great question in terms of this pandemic time, I would answer your question in two different ways. One would be that specifically during the pandemic time, and then apart from the pandemic in general. So during this pandemic time, even before the first cases of coronavirus was here in the US and around the world, I started raising awareness about some steps from a public health perspective, from my personal experience in treating patients at the clinical level. I was trying to raise awareness and make sure that people are prepared for a day, which is going to be unfortunately overwhelming for a lot of hospitals and physicians, and healthcare facilities. So during this pandemic time, people need to be proactive, especially the decision-makers and people who are running hospitals and running healthcare facilities. By proactive, I mean that one of the things that they need, as I mentioned, was the PPE. So they have to be prepared to have enough of the PPE at their facility, they have to make sure that they have enough people on the ground, by people, I mean, healthcare professionals, so that they can have different shifts. Because the burden is way more than the regular days, and if a physician or any other healthcare provider is staying in the hospital, instead of eight hours, 12 hours, that definitely they need to rest. So in order to rest, they need to have the next shift, like if they can have different shifts, instead of two shifts, or three shifts, making sure that they have enough people in different shifts so that they can have the virus under control, they also make sure that their healthcare providers have time to rest.
Dr. Manon 32:36
But just to interrupt you here, so you’re looking at it, though, from a public health perspective, which is what you’re in, I totally get that. And so that’s more what administration can do. What can the doctors or the nurses do when they’re in the situation that they’re in?
Dr. Hamid Elmyar 32:57
That’s a great question. And I wish I had all the answers for them. And I admit that I don’t have all the answers. That’s why I believe in collaboration, and I have a whole team of professionals and I am really interested in working collaboratively to have a package, holistic package, if it’s for the public, if it’s for healthcare providers. And for healthcare providers, of course, one thing that is really important I want to mention here is that as healthcare providers, or physicians, we always think that, oh, we know this, this is a problem, this is a disease, but we never think about solutions. We take it easy, or we ignore it. Sometimes, unfortunately, it’s a stigma, that a healthcare professional or a physician complains about burnout or complaints about other issues that they are seeing on a daily basis. And that is, I think the main reason that my focus is on health care providers and the main reason why a lot of them don’t get the necessary help that they want. Because, unfortunately, a lot of people would be just, oh, this is in capability, you’re not capable of doing your work, you’re complaining and all that. But to go back to the life, work balance. If a physician is not taking care of his or her own health, how can he or she be able to take care of other people’s, their patient’s health? And for that to happen, I have a group of experts from medical doctors to naturopathic to functional medicine physicians to psychologists, clinical psychologists to other public health practitioners, other health practitioners who are working from neuro biofeedback. And what really happens is not necessarily just what we read in the textbooks, because when the burden, that burnout happens, it has many actually reasons. And I noted, actually, a few important points here, I wanted to mention that the best one is the MBI. And based on their definitions, burnout is, according to treat, has three components. Emotional exhaustion, depersonalization, and reduced personal accomplishment. So when we think about these important three measures, three components, it doesn’t really…writing a prescription is not the solution. So for that, I have a package of whatever is needed there. And that will be on my panel discussion.
Dr. Manon 36:08
I very much look forward to listening to that panel discussion and see what happens with that, because I think it’s very much needed. I think too, it’s having a platform for discussion, which is very important, because what at least my observation of this pandemic, which is not a popular spoken view, but it does seem that there’s been a lot of doctors and healthcare people speaking out saying, ‘Hey, you know, in this hospital, they’re’ using zinc or and vitamin D, and they have high vitamin C injections’. And it’s like, there’s nothing, no coverage, no media, no nothing. And the doctors who are involved in that are seeing results that they want to talk about there. They’re not massive studies. But it’s like, there’s a desire when you go into the profession to help people you want to help people. And it’s like if you’re doing something that seems to have an impact, it needs to be further studied and looked at, but it needs to be shared. And the same, there was I remember, a sample of the doctors speaking out as well when they didn’t understand the nature of the virus, and they were using these, intubation, and the respirators were actually at fault. That no one’s at fault, because we’re all just learning at, I get that. But the point is, there wasn’t a voice, there wasn’t a place to share those concern or those observations, and not being in practice right now just noticing all of this, it’s a huge stressor when there isn’t a real genuine platform for caring about people, and how it works. And it seems so vested in people and industries that have so-called solutions, whether it’s the vaccine or this. I mean, it’s not that there isn’t much money to be made, which seems to be what runs a lot of this. But the doctors and nurses and health care practitioners are, I don’t feel are getting their voice heard. And it’s not safe for them to share. And that’s what I find the most scary.
Dr. Hamid Elmyar 38:46
Yeah, of course, I agree with you on all of it. And this pandemic was, you know, pandemics don’t happen every year and that’s not the type of disease that we were seeing on a daily basis as healthcare practitioners. And of course, it was new, and it’s still new. It’s been already a year into this coronavirus pandemic and we are still learning. So when something is new, a disease is new, a virus is not known, there is no medication, there’s no vaccination for that. Obviously, the impact, the negative impact of that virus is way more than a virus or a bacteria which is known. If we know if there are some bacteria we have medication for it, so we know what protocol should we use, what to tell for the patients, and how long would it take, what kind of medications are we prescribing? And, but this was new, so that’s another story.
Dr. Manon 39:54
I think the fact that it’s new, they’re separate things to me. And that’s why I love the idea that you have a platform where medical professionals can actually talk freely about what they saw, what they’re experiencing, what’s going on because I do think that as a collaboration, they’re in the best position to see what’s going on. And we know very well that these numbers, they’ve gone from crazy to nothing, then tests, then there’s questions about tests, and it just keeps going and going, and it’s very confusing for the public. But as a health care professional in it, it’s so important, I think, to have that freedom to talk and see what’s happening in a ‘free’ way. I’m trying to think there’s a group of I think it’s 40,000 doctors now who have signed together to collaborate. I think the name of it, it’s escaping me, of course. Oh, goodness. I think it was started in Germany, but for that very same reason, let’s have frank discussions, you know, but that’s more to do with this particular pandemic. I think the question you’re raising is also a general one, you know, what motivated your life from going into public health?
Dr. Hamid Elmyar 41:31
I just mentioned briefly that I wanted to focus on both sides during this pandemic, and then on in general. The general part was that in the package I mentioned that because we need a holistic approach, we need a collaborative and more systematic approach when it comes to burnout. Or during other regular days, because the burnout is not a problem only during a pandemic, of course, in a pandemic, it increased, but it’s an ongoing problem.
Dr. Manon 42:11
Definitely. Okay. Well, I mean, our time, I can’t believe it’s already over. I feel like we can have many discussions. So any last words you want to leave everyone with before we close?
Dr. Hamid Elmyar 42:32
Yeah. And first of all, thank you for giving me this opportunity to be on this platform and share my experience with you and with your audience.
Dr. Hamid Elmyar 42:43
So the message is most of the belief that I have is that health is not limited to private practices in hospitals. It has to start from every individual communities, school systems, everywhere. And for that to happen, we need to raise awareness, we have to look for those underlying causes and root causes. And we have to have a collaborative, systematic approach to health in order to save people’s lives. Also, not only helping our communities but health care professionals themselves as well.
Dr. Manon 43:22
All right, okay. Well, thank you very much, and it was lovely to interview you.
Dr. Hamid Elmyar 43:28
It’s been a pleasure. Thank you for having me.
Thank you for joining us. For more information, go to DrManonBolliger.com.